Sincere Thanks
In Feb 2014 I set about starting a physiotherapy degree. I was accepted to study at both AUT and University of Otago. I selected Otago. Fast forward some great years to 26th May 2017; I finished my last day of placement for the BPhty degree. It's now August 2017, I've registered as a physiotherapist (I'm a physiotherapist!!) and I've been working a few weeks and it's time to graduate!
112 blog posts!
Many, many hours of blogging.
Every week of study for 2014, 2015 & 2016 blogged!
Overviews of repeated papers in 2017 blogged!
Parents and friends kept up to date!
What a success!
Here we are, the big day.
The moment that we were all looking forward to from day one.
Graduation!
So let me dedicate this last post to all those that have helped me get to the starting line of my career in physiotherapy.
- Family, in particular my parents Sheryll & Ted! I'm indebted to you in every sense of the word.
- Flatmates in my first year of physio. Gillian Tan, you're a legend. Lets keep in touch.
- Physio peers! Shout out to Chris Pett, we haven't gone tramping yet mate! My peers, you're all great!
- School of Physio staff. Clinical, educational and administrative. Each of you were very supportive and shared a personal level of kindness. They also keep us students up to date with research via Twitter: @Rammani79, @HemDevan, @danielcr, @alexmacz, @DrGiselaSole, @ChrisHiggsPT, @PhysioDean, @catchapplePT
- Knox Rehabilitation Clinic staff. Stacey & Katie, the best chiropractor and massage therapist (respectively) in NZ. (If other massage therapists think they are the best, invite me along to a free hour session and I'll let you know where you sit ;) )
- Leon Mabire. Yep, you get a special mention! Follow on Twitter @LeonMabire
- Clinical supervisors, clinical educators and other physiotherapists!! Being a student isn't easy, but you all helped foster a culture of excellence in us all. I know there will always be struggles in the dynamics of healthcare, but from what I observed - you should hold your head up high.
- Flatties in Nelson. Jenna, Nicolas, Valerie & Darren, oh and the neighbour's dog Borris.
- Sabella & family. You've brought balance and direction to my life.
- Joyce & family. I'm grateful for the journey we shared.
- Hannah, Marnie & Wayne, the quiet cheerleaders in the background!
- Good friends; Brendan, Candice, Stuart, Bella, Alice, Mike and co. The rocks in my life!
- Mike & Heather, for your kindness and hospitality during PSW weeks in CHCH.
- BPhEd Staff and classmates: you ultimately got me into the PT programme!
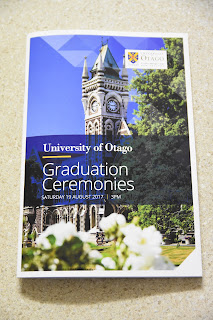
Graduation
Graduation for physiotherapists usually takes place in December, where they give out special awards and have formal gatherings. Graduating in August is low-key. We're the odds n' ends students who had to repeat a paper or two... But that's fine, we made it. We've met the standards just like every other physio out there. Congrats to us - we are just as deserving!The graduation ceremony is held at the Dunedin town hall, preceded by a graduation march down the main street of Dunedin led by the Dunedin City Pipe Band. Academic regalia is hired for the occassion. The UoO physiotherapy hood colour is Peacock Green. The University of Otago and Dunedin have many picturesk locations to pose with family and friends; the top three places to have a picture taken would be at the clock tower, at the UoO signage in front of St Davids lecture theatre, and in front of the physiotherapy department.
Photos of graduation
 |
| Proud parents! |
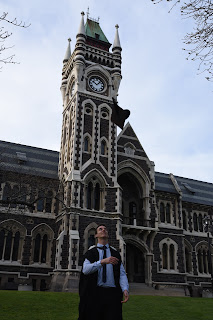 |
| What not to do ;) |
 |
| Leigh Hale (Dean of School of Physio) and I at the graduates brunch! |
 |
| Graduates parade, lead by the Dunedin Pipe Band. |
 |
| Capping show |
 |
| A photo that includes very prestigious physio faculty staff members and alumni |
 |
| Physio Celebrities (Margot Skinner and Stanley Paris) |
Stanley Paris, the distinguished guest speaker at the graduate ceremony. spoke about his up bringing in Dunedin and study at what would become University of Otago School of Physiotherapy. He has had an entrepreneurial career, starting from door knocking to sell fire wood with a 300% price markup at the age of 7 years, to establishing three universities of health sciences in the US. Stanley embraces a challenge, takes calculated risks and is not afraid of failure. He is considered the grandfather of manipulative therapy in physiotherapy.
 |
| An expensive piece of paper! |
 |
| A fancy ticket holder 'ticket wallet' |
Becoming a physiotherapist
To legally call yourself a physiotherapist, you have to have a recognised physiotherapy qualification, be registered as a physiotherapist, and have an annual practicing certificate.Registration process ($230)
- As soon as (or even one week before) you finish your last placement you should consider applying for your criminal record which is required to register as a physiotherapist with the Board. It can take a long time for the process to be completed (the website states 20 days). You can do this via email here: https://www.justice.govt.nz/criminal-records/get-your-own/
- If you don't get your request within that period, give them a ring or follow the process outlined here: https://www.justice.govt.nz/criminal-records/contact-us/
- Applying for your transcript is easy, either wait until you graduate (you'll receive a copy with your Bachelor's certificate) or you can apply (at a cost) on the university website here: https://secure-www.otago.ac.nz/study/transcripts/
- You will need to download the registration form from the NZ Board of Physiotherapy website here: https://www.physioboard.org.nz/new-zealand-qualified-physiotherapists
- A section in the registration process requires you make a statutory declaration with a justice of the peace or similarly qualified person. They can sign the copy of your certificate / transcript as legitimate and passport / birth certificate at the same time. nb. there is a guide to registering on the board of physiotherapy website which is very helpful for NZ new physio graduates.
- Pop the completed documents in the mail addressed to the board (address is on the Board of Physiotherapy website).
- Begin this once you've registered or send in the application along with your application to register.
 |
| License to Touch! Annual Practicing Certificate (APC) |
Jobs!
Most students finish their degree having networked and aware of job vacancies. Some are offered jobs before they finish the degree. Others who decide they want to work in a different region of New Zealand will need to go about finding a job the old fashioned way. nb. you can apply for jobs whilst in the registration process (or even if you haven't begun the registration process), just know that in order to practice physiotherapy you will need to have a practicing certificate - let your prospective employer know that you're in the process of obtaining this. They might offer you a contract with a clause to this effect.- NZ Physiotherapy Jobs
- Physiotherapy New Zealand
- DHB Career websites
- Trademe Jobs
- Get out there, browse for prospective clinics and fire through your CV and a cover letter.
- When you've got yourself an interview, dress to impress.
- Treaty of Waitangi principles, what are they and how have you used these principles in your practice.
- MSK and Respiratory case study: you will be given two case studies, in my case one was MSK and the other was respiratory focused. The cases I had, had problems to identify e.g. an incorrect Drs diagnosis or what was truly intended by the term 'wheelchair bound' and it had medical complexities to consider e.g. a person with MS with a respiratory presentation. The structure of each case question was open e.g. talk us though your subjective and objective assessment. How would you proceed to treat them? How would you know they were ready for discharge?
- Discuss a recent article you read. I printed the article out and brought it along. It turned out that one of the physiotherapists interviewing me was familiar with the article authors and that particular article I presented.
- Why do you want a job with the DHB? What qualities do you bring to the position, you're asked to then sell yourself...
- How would you handle a very heavy caseload, what would you do? How would you prioritise patients in a stressful environment?
Overview of my private practice job interviews
- These are a whole lot less formal. The balance is shifted from you selling yourself and proving your competencies, toward the clinic director/principal selling you reasons why you should work with them (depending on the number of applicants they have got).
- In my experience (n=2 interviews) you will have a discussion to find out about their philosophy of physiotherapy in their practice, and how it fits with your philosophy/views/values.
- You'll find out what they offer their practitioners; regular 'catch-ups', professional development. They may also ask what you expect from them as a potential employer.
- You'll discuss your interests and what additional things you can bring to the clinic (e.g. do you want to work with a sports team).
- They will most likely ask whether you're familiar with their client notes software e.g. Gensolve seems to be pretty common.
Choosing a job
Things to look for in a private practice
- Supported professional development: regular in service training, contribution to short course costs (e.g. dry needling or McKenzie/Mulligan courses)?
- Will they reimburse you for your annual practicing certificate?
- Do you get some 1 on 1 mentoring each week or is there an open communication culture where you can pop your head in to the clinic directors door and ask questions?
- Do they sell products (braces, orthotics, massage oils etc) or services (complimentary massages, personal well-being programmes)? Get them to tell you about how they work and how they would fit into your practice? e.g. will you have to be continuing to sell products/services to patients? Do they have additional charges for taping or dry needling?
- What do they charge per patient vs how long do you get with each patient? The standard seems to be 40min for a new patient and 20min for a follow-up appointment. Do they have additional costs for patients to see a more experienced practitioner or are all physiotherapy services seen to be of equal high standard (and the cost reflected by this). Are you expected to achieve a minimum amount of treatments per client target?
- What patient presentations do they usually treat? What contracts do they hold with ACC?
- What are your hours? Do you work weekends?
- Are you expected to pick up work with a sport team or provide a community pilates class?
- Do they have a physiotherapy or clinic philosophy?
- What relationships do they have with other clinics in the area? Do they have good relationships with GPs or surgeons?
- Who works there, what are their qualifications / clinical background? Listen to their 'physio talk' - what schools of thought do they follow? muscle imbalance and ultrasound? Barefoot? Do they have a bias toward one manual therapy theory?
- What facilities do they have in the clinic? How does the clinic environment feel when you walk in the door for the first time?
- What software do they use for note taking? Uniform provided?
- Do they have parking space or a space to house your bike (depending on how you plan to travel to work)
- Are they accessible to older persons and people with disabilities?
- ...Physio is a small profession, and clinics get a reputation for their good work (and their blunders), so ask around!
Physiotherapists are passionate about their job. It doesn't pay the most, additional hours are often worked above and beyond that specified in the contract, we continue to write a portfolio (yikes!), but we are passionate about health, wellbeing and movement. Repeating two papers allowed me to see what the next cohort of students were like, and it's fair to say that they are equally passionate. If you share a similar passion, then physiotherapy is a career for you!
Whether you get an email from the University of Otago like this:
Or a letter from AUT University like this:
Then, good on you! You're a winner!
It's now time to start paying off that student loan (Useful Budgeting Link) and making a difference in people's lives.
Many thanks. It's been a great adventure.
Phil Butler, BPhEd, BPhty.
Physiotherapist, outdoor enthusiast & blogger.
@PhilNZ10
Inspiration to be physically active: https://500px.com/philipbutler/
Future blogs may appear here: https://physiopotential.blogspot.com